Blood clotting, or thrombosis, is a protective mechanism that occurs naturally to prevent excessive bleeding when the body is injured. It can become a problem, however, if blood clots form in veins and obstruct proper blood flow. When this occurs it can lead to superficial thrombosis, or in more serious cases, deep vein thrombosis. But while the condition can’t be cured, per se, it can be managed and treated.
What is Deep Vein Thrombosis?
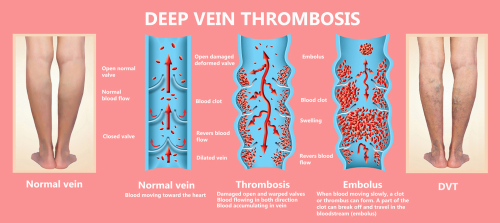
Deep vein thrombosis occurs when a blood clot (thrombus) forms in a deep vein; ie., one of the large trunk veins in your muscle or bone that connect your heart and lungs with the superficial “surface” veins all over your body. When a clot like this forms, it can have varied health effects depending on where it occurs. Thrombosis may be a singular incident or a more chronic problem. However, the good news is that there are ways to minimise your risk and even treat the condition.
What causes Deep Vein Thrombosis?
Factors that increase your likelihood of developing DVT are similar to those for other vein diseases. Below are some causes of DVT:
- Age
- Damage to an artery, vein or surrounding tissue
- Surgery
- Limited movement: extended periods of sitting or lying, such as travelling in a plane or car for a long time, convalescing in a hospital bed or having your leg immobilised in a cast.
- Genetics: A family history of DVT, pulmonary embolism, or blood-clotting disorders can leave you prone to developing a clot, so make sure you’re taking care of your veins.
- Pregnancy (especially in the later stages and for up to six weeks after birth) increases your chances of developing a clot, so keep moving and wear compression stockings.
- Medications like the pill and hormone replacement therapy usually increase your body’s ability to clot and develop a DVT.
- Being overweight or obese puts increased pressure on the veins in your lower half.
- Smoking increases your risk of DVT and blood clots, as well as a range of other health conditions. Speak to your GP to find the best way to quit for good.
The question of whether having varicose veins is a significant risk factor for DVT is more controversial because a clear cause-and-effect relationship has yet to be firmly established. However, in a study reported in the German journal VASA, researchers found that 5.6% of patients with varicose veins developed DVT, compared to 0.9% of the control group without varicose veins. They also found that those with varicose veins, who also had a history of previous venous thromboembolism or recent hospital discharge, were even more at risk.
Symptoms of DVT: What does Thrombosis feel like?
Clots can cause pain in the leg, like a cramping soreness, as well as redness and warmth in the area. Other symptoms of DVT include:
- A persistent, throbbing, cramp-like feeling in the leg
- Pain and tenderness in the leg when standing or walking – most often the same type of pain as a severe muscle cramp.
- Swelling in the affected area, often with redness or discolouration of the skin.
- Warmth in the affected area.
- Altered mobility of the leg. If you find that bending the foot or knee causes more pain, it can be a sign of a DVT.
In some cases, a deep vein clot may dislodge and travel to the heart or lungs, causing pulmonary embolism. In this case, you may feel:
- Shortness of breath, especially if it gets worse after exercise.
- A cough that produces bloody sputum or pink, foamy mucus.
- Fever or excessive sweating.
- Clammy or discoloured skin, often accompanied by feelings of anxiety.
- Sudden lightheadedness, dizziness, or fainting.
- Rapid or irregular heartbeat.
- Sharp chest pain gets worse when you cough, breathe deeply, bend over or stoop, and doesn’t go away when you rest.
If you are experiencing any of these symptoms, seek medical help IMMEDIATELY. Even if the DVT hasn’t yet dislodged, it’s essential to catch it and dissolve it early to prevent the risk of pulmonary embolism, as the latter is a life-threatening condition. To dissolve the clot, a medical practitioner will often prescribe an anticoagulant.
What is the risk of having a Thrombus, or blood clot?
The primary risk of thrombosis is that it breaks loose and travels through your bloodstream. This can cause it to lodge in your lungs, blocking blood flow and causing a pulmonary embolism, which can be life-threatening. (If you start to experience sudden shortness of breath, chest pain, rapid pulse, light-headedness/dizziness or coughing up blood, seek immediate medical attention.)
Another risk of thrombosis is developing Postphlebitic Syndrome (PTS). This occurs when part of the leg is damaged by a DVT, leading to long-term swelling, pain, skin discolouration and the forming of ulcers.
DVT is relatively uncommon, affecting about 1 in 1000 people (Anyone over 80 is 10 times more likely to develop a DVT). If you suspect that you have one, it’s important to see a doctor to diagnose and refer you for appropriate treatment.
Read more: Why do blood clots form?
Can thrombosis (DVT) be cured?
Unfortunately, there’s no cure for blood clots. Even if one is treated, another may form down the line, especially if you’re predisposed to the condition or sustain an injury. However, there are several simple and successful methods used to treat DVT and other thrombi. While we’ve outlined some key remedies below, they should always be done in consultation with a doctor.
Anti-Coagulants
Known as blood thinners, this deep vein thrombosis treatment reduces the risk of a clot forming and helps your body safely remove most clots that have formed. These should only be taken with the consultation of a doctor.
Compression Stockings
Medical-grade compression stockings are one of the most effective ways to minimise the risk of clots forming, and are particularly effective at treating current clots, especially alongside the use of anticoagulants. Wearing compression stockings on flights, while driving, and while at work (if you stand or sit all day), will help to reduce the risk of clots forming, and is one of the best ways to manage the chronic forming of clots.
Exercise and Therapy
This is recommended to be done in combination with compression stockings. By exercising regularly, even if it’s just a simple walk, your circulation improves, helping the blood move properly. Sometimes, a doctor will recommend physiotherapy and stretches to help improve circulation and manage any associated pain, as well as reduce the risk of further clots (particularly in people who are overweight).
To determine your own risk for DVT, ask your specialist at The Vein Institute. They can diagnose the presence of blood clots using Duplex ultrasound or venography (injecting a dye into the vein that then reveals blockages in X-rays). Your vein doctor can also recommend diet and lifestyle changes to reduce your DVT risk if your risk level is high for hereditary or other reasons.
Seek expert advice
The doctors at The Vein Institute specialise in varicose vein treatment. We offer patients a comprehensive program using non-surgical laser treatment techniques. To book a consultation and discuss our treatment program, call 13 VEINS (that’s 13 83467) or enquire via the Contact Us page.