Vein conditions should always be considered serious. Issues with your veins can cause poor blood circulation, and could therefore lead to health concerns everywhere from your skin to your heart. We do want to note that there are some people with varicose veins who live with them for many years without experiencing any serious side effects. But not everyone is that lucky. In a large percentage of cases, the side effects caused by varicose veins do get worse without treatment.
How bad can varicose veins get?
One of the things to remember if you have varicose veins is that they are a circulatory disorder. The tiny valves in your veins that were supposed to keep blood flowing up towards the heart are damaged by a condition called chronic venous insufficiency, or CVI. As a result, over time your circulation may become worse and worse, causing changes in the colour and texture of your legs.
Generally, vein specialists list the following stages through which vein disease progresses in most people.
Stage 1: Spider Veins
Spider veins are tiny dilated blood vessels. They’re usually 0.5-1 millimetres in diameter and are red or purple in colour. These veins usually pop up in clusters that look like spider webs, thus the name. While many wish to get rid of these veins for cosmetic reasons, they’re rarely a cause for concern.
Stage 2: Varicose Veins
Varicose Veins are bulging twisted veins often accompanied by symptoms of pain, itching, swelling, and limb fatigue. Although not everyone experiences these symptoms, they are likely. And unfortunately, even if you don’t have them now, they may develop over time.
Stage 3: Oedema
This is essentially an advanced stage of swelling. If varicose veins are left unaddressed for too long, overflowing veins and excess fluid build-up may become chronic.
Stage 4: Skin changes
Varicose veins affect the skin in a few key ways. With slowed oxygen and nutrient delivery, your skin won’t get what it needs to stay strong and healthy. So, along with a sheen, you may start noticing redness and inflammation, discolouration (known as hyperpigmentation), and a tough, leathery texture that makes it prone to breakage and infection.
Stage 5: Venous ulcer
A venous ulcer is a chronic wound. Due to the skin not getting enough nutrients, this open sore is extremely slow to heal and difficult to treat.
Not everyone with a spider or varicose veins will progress through all of these stages. Experts don’t know exactly why some people do more than others. They can see a strong hereditary component in this process but it is not the only factor. Careers with prolonged standing or sitting, excess weight and smoking are also factors that could progress vein disease. While all varicose veins should be evaluated by a specialist, it is particularly important if you have a family history of progressive venous disease or if you have swelling, pigmentation or an ulcer.
What other dangerous conditions can varicose veins cause?
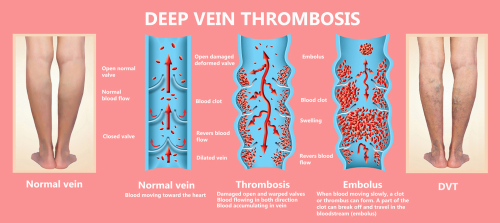
Although there is not a direct cause-and-effect relationship between varicose veins and the development of blood clots (thrombi), the same genetic conditions that increase varicose vein risk are also inherited and make thrombosis more likely. Blood clots may form in the superficial (close to the surface of the skin) veins, leading to a condition called superficial thrombosis. It first manifests as a red streak along the affected vein, which then often escalates to inflammation (phlebitis), which leaves the veins feeling warm, tender, and swollen. This condition is typically more annoying than dangerous because there is little danger that the clots will break up and travel elsewhere in the body.
A related and far more dangerous condition is called deep vein thrombosis (DVT). If DVT occurs, blood clots begin to form in the deeper, larger veins further below the surface. If these blood clots break loose, they can travel to the lungs (where they can cause a pulmonary embolism) or to the brain (where they can cause a stroke). Both conditions can be life-threatening.
How can I reduce the risk of varicose veins progressing?
The first option is lifestyle changes, which we’d recommend if you have varicose veins but aren’t yet experiencing uncomfortable symptoms. Depending on your doctor’s recommendations, these may include the following:
Exercise
This is a great way to boost circulation and improve muscle activity. Unlike your arteries (which only need the heart to propel blood through them), the veins rely on muscle movement. So, make sure to do plenty of walking, take breaks between long hours of sitting or standing, and do some strengthening exercises.
Compression
Compression stockings are a good way to improve circulation even when you’re still. They gently stimulate and squeeze the muscle to keep blood moving into and up the deep veins.
Healthy diet
Eat plenty of fibre to avoid straining the abdominal and deep veins. You should also make sure your diet has plenty of vitamins and flavonoids to keep your veins strong.
To reduce the risk of DVT-causing problems specifically, it’s best to speak to a doctor, look at blood thinners and other medications, and use compression stockings.
When should I get treatment?
You should get varicose vein treatment ASAP if you start experiencing symptoms of pain, swelling, or changes in the colour of your skin. The sooner you get treatment the better. These are not merely cosmetic problems that will go away on their own. The higher levels are more difficult to treat and may take longer to resolve. In particular, ulcers, which are the result of chronic and untreated leakage from varicose veins.
If you’re concerned about your veins, or if you’ve let your varicose veins go untreated for a while, we advise getting a scan and venous health evaluation. There are effective treatments that will help minimise your symptoms, improve your circulation and get you back to your best.
Give us a call at 13 VEINS (that’s 13 83467) to book an appointment.

