Varicose veins are common and whether you’ve got a vein or two, or a full network from toe to thigh. Managing them effectively can make a big difference in your vein health and overall level of comfort. Knowing what is helpful and what could make the condition worse can be confusing. To help out, we’ve come up with six dos and don’ts for varicose veins that will help to reduce discomfort and find treatment.
Firstly, what are varicose veins?
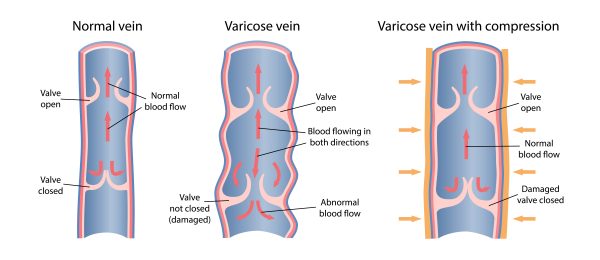
Varicose veins are twisted enlarged veins generally occurring in the legs and feet. They affect up to 30% of the Australian population and often appear blue or dark purple in colour. They develop due to damaged vein valves which are no longer able to sufficiently circulate blood back up to the heart.
Some people experience no symptoms at all whilst others may experience all, or some, of the below. In general, vein pain is considered vague and dull rather than sharp or immediate. If you raise your legs and the pain goes away, this is an indication your pain is vein related.
- Pain, itching or heaviness in the legs.
- Burning, throbbing or muscle cramping.
- Pain that intensified after prolonged sitting or standing.
- Chronic swelling in the lower legs or ankles.
Do’s and Don’ts for Varicose Veins
1. Exercise for varicose veins
Do: Exercise regularly, walking, swimming, cycling are all great low-impact exercises that get the circulation moving properly. Focus on smaller periods of activity more regularly and build up from there. Read more: Exercise & varicose veins.
Don’t: Over-strain yourself. As tempting as it is to push yourself, if you’re lifting heavy weights or engaging in high impact activity, you can actually damage the veins and do more harm than good.
2. How diet influences veins
Do: Maintain a consistent diet which is low in sugar, fat and cholesterol. And high in fruit and vegetables. This will help to keep your veins clear and strong. Download the Australian Governments’ dietary guidelines booklet.
Don’t: Go in for fad diets. While many promise quick results, healthy eating avoiding sugar and fat is the best thing for your veins. If you have other weight problems, speak to your GP to manage weight loss alongside vein health.
3. Medical Advice for varicose veins
Do: Speak to your doctor. Your GP is your main guide and best resource for your general health. They can also provide a referral to a vein specialist or Phlebologist who will conduct a venous ultrasound to determine the source of the varicose veins as well as provide a recommended treatment plan.
Don’t: Listen to speculation. While our friends can often have helpful tips for many parts of our life, it’s important to leave medical advice to the professionals. Your health is the most important thing you have, so take care of it accordingly.
One common misconception is that varicose veins are simply a cosmetic or superficial concern. In many instances varicose veins are harmless, however, veins become varicose due to a condition called Chronic Venous Insufficiency. When CVI occurs, blood isn’t being properly circulated back up to the heart. It is therefore important to speak with a doctor and have any vein issues assessed. Read more: How damaged vein valves impact your health.
4. Compression stockings
Do: Wear medical grade compression stockings. It’s important to use medical-grade compression in the treatment and management of varicose veins to restore vein health and boost circulation.
Don’t: Go for fashion first. There are many brands that have compression pants that look trendy and seem fashionable, but they don’t provide the medical compression needed. If you’re wanting compression while still being fashionable, check out Bauerfeind’s VenoTrain Micro, with a light weave and breathable fabric, you can wear them underneath your other clothes, so you get the best of both worlds.
5. Lifestyle choices
Do: Keep active. If you work at a desk, drive a lot or have something else that’s got you sitting for a long time, then it’s important to keep moving over the day. Get up every 20-30 minutes and move around a bit. Quit smoking. The main culprits in tobacco smoke are carbon monoxide and nicotine. Both of which have been shown to restrict blood circulation, particularly to the legs. Read more: Can vaping and smoking cause varicose veins?
Don’t: Stay on the couch. Even though it’s nice to rest after a long day’s work, keeping active over the day and night helps a lot in preventing varicose veins forming.
6. Do’s and don’ts for varicose veins treatment
Do: Seek treatment. You may have heard of surgical stripping – an in-hospital surgery to remove varicose veins from the legs. It requires a long hospital stay and a lengthy recovery. Modern non-surgical treatment options, like those offered at The Vein Institute, are minimally invasive and can be done on your lunch break. Learn more: Varicose vein treatment.
Don’t: Look for the silver bullet. Varicose veins change from person to person, and the treatment is best done by combining a range of remedies for the best overall solution.
Read more: Does crossing your legs cause varicose veins?
Seek expert advice
The doctors at The Vein Institute specialise in varicose vein treatment. We offer patients a comprehensive program using non-surgical laser treatment techniques. You can learn more in our Definitive Guide to Varicose Vein Treatment.
The benefits of non-surgical varicose vein treatment are:
- Walk-in walk-out treatment
- 98% success rate
- Extremely effective
- Can be performed at a clinic (no hospitalisation)
- No general anaesthetic
- Medicare rebates apply
- No downtime or time away from work
To book a consultation and discuss our treatment program, call 1300 981 402. Or, make an enquiry via the Contact Us page.