What are varicose veins?
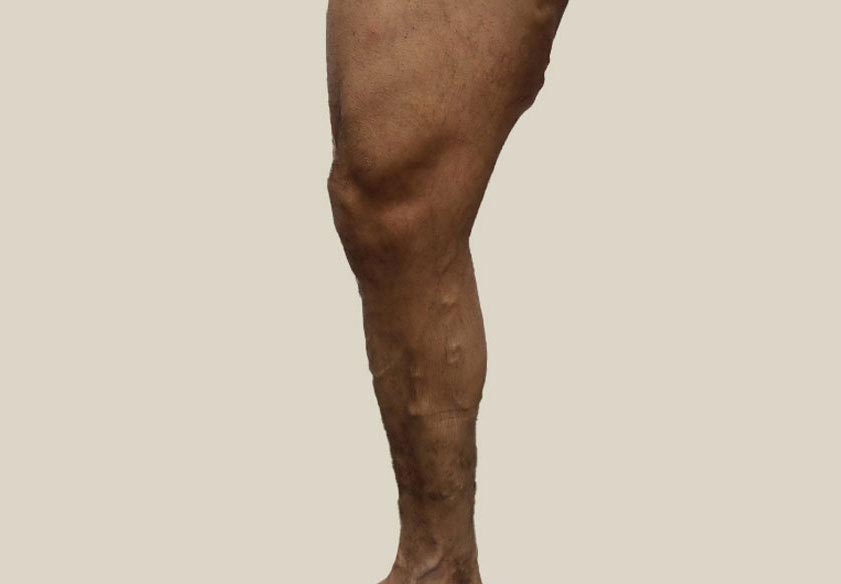
Varicose veins are twisted enlarged veins that commonly protrude above the skin. They are usually easily identifiable due to their twisted and discoloured nature. However, they are not always visible to the naked eye. The veins become enlarged when the valves stop functioning and the deoxygenated blood starts slipping through and pooling in the vein, hence their trademark bluish-purple colour.
In some cases, varicose veins are a cosmetic concern. But in many, they progress into a medical issue.
What are the symptoms of varicose veins?
- Pain in the legs. Typically, this will be a dull ache that lessens when you elevate your legs at or above heart level.
- Itchiness around the affected area. Itching is often caused by varicose eczema, which turns the skin hard, dry, and flaky.
- Swelling. In the early stages, swelling may come and go – worsening as you sit or stand for long periods and improving once you elevate the legs or exercise. In later stages, it may become chronic.
- Burning sensations. This may be the result of varicose eczema. It can also be caused by the veins swelling and agitating surrounding nerves.
- Cramping. As blood pools, oxygen and nutrient delivery to the muscle slows, causing cramps.
Some people experience no symptoms at all while others may experience all, or some, of the above.
What causes varicose veins?
Varicose veins are caused by Chronic Venous Insufficiency (CVI). When the valves in the veins stop working properly, blood starts slipping backwards and pooling in the vein instead of travelling up to the heart. The condition is primarily genetic, but there are a few other risk factors that come into play:
- Pregnancy can cause varicose veins due to higher levels of progesterone, an expanding uterus, and increased abdominal pressure.
- Menopause also causes hormone fluctuations that affect the vein walls.
- Age slowly weakens vein walls and valves.
- Obesity puts veins under increased strain.
- Your profession can cause varicose veins as long hours of sitting and standing mean the calf isn’t helping the veins pump blood up to the heart.
- A sedentary lifestyle and a bad diet mean your veins aren’t getting the nutrients or muscular help they need.
Where can varicose veins appear?
Varicose veins can appear anywhere there are veins on your body, including arms, torso, genitals, and legs. However, it is more common to get varicose veins in the feet and legs, as these veins are under more daily strain. They have to fight against gravity and have a long way to pull blood to the heart.
Can I prevent varicose veins?
While you can’t prevent the condition with absolute certainty, there are steps you can take to minimise your risk:
- Stay active and exercise regularly
- Keep your weight within a healthy range
- Eat a high-fibre and low-sodium diet
- Take frequent breaks to move if your job requires standing or sitting for prolonged periods
- Avoid wearing constrictive clothing such as skinny jeans
- Elevate your legs for a few minutes after work
Do I need to treat my varicose veins?
If your varicose veins pose little discomfort and health risk, then treatment may not be necessary. However, some patients find varicose veins unsightly and wish to have them addressed for aesthetic reasons.
If you’re experiencing varicose veins or symptoms, or have a family history of the disease, it’s a good idea to see a professional vein specialist for an assessment. They will advise you whether treatment is recommended and go over all the treatment options with you. Please note that even if your varicose veins aren’t causing much discomfort now, the condition may worsen over time. It may even cause more dangerous health complications such as:
Other conditions
Bulging veins
Veins which bulge and protrude above the skin are not always a medical concern. Bulging veins sometimes appear on the arms or legs during exercise. These veins are also often seen on our hands and feet, and become increasingly common as we age.
Reticular veins
Smaller than varicose veins, reticular veins are visible however they do not protrude above the surface of the skin. Due to being filled with deoxygenated blood, the veins appear blue or purple in colour, they are most commonly found on the inner thigh, the backs of knees, or on the ankles.
Spider Veins
Spider veins are the mildest form of venous insufficiency. The tiny, string-like damaged veins, can appear on the surface of the skin. These are most typically found on the face or legs and can be flat or slightly raised and form under the skin as wavy lines, webs or branches. They can range in colour – from purple to red.
Varicose Veins in Feet and Ankles
Varicose veins (and spider veins – less severe forms of varicose veins) around the feet and ankles are referred to as Corona Phlebectasia by vein specialists. Statistics indicate that 3 out of 10 people will experience varicose in their adult lives. Most importantly, symptoms can differ in severity, ranging from strictly cosmetic to indicating a more serious medical problem.
Pelvic Congestion Syndrome
Pelvic congestion syndrome (PCS) is chronic pain affecting women. It can be incredibly debilitating and may even lead to disability. PCS pain is frequently confused for menstrual pain, so it’s important to know the symptoms of pelvic congestion syndrome, as well as the causes and available treatment options. PCS affects the pelvis region (lower torso) and is associated with the pooling of blood in the veins of the pelvis, which have become dilated, swollen and distorted.
Lymphoedema
Lymphoedema, or poor fluid drainage from the lymphatic systems, is swelling that is caused by a collection of too much lymph fluid. It usually happens in your arms and legs, but is not uncommon to occur in other places of the body. This swelling may cause pain and limit how well the affected area moves. Lymphedema can be a result of damaged lymph nodes from cancer treatment and a result of infection, injury or trauma of areas of the body.
Varicose Veins Treatments
Endovenous Laser Ablation
Endovenous laser ablation (EVLA) is a minimally-invasive laser treatment for varicose veins. Over the past decade, this procedure, along with Radiofrequency ablation (RFA) have emerged as the gold standard treatments, due to their high success rates, short recovery times and minimal discomfort for patients.
Radiofrequency Ablation
Radiofrequency ablation involves inserting a catheter into the vein then delivering a source of heat, closing off the vein and stopping the flow of blood. During RFA treatment, radiofrequency energy is administered in 20-second bursts directly into the vein through a tiny catheter. Rather than clotting the blood, the radiofrequency energy targets the collagen in the vein wall, causing it to shrink and prevent blood from circulating through that vein.
Medical Superglue VenaSeal
VenaSeal is an advanced new treatment for venous insufficiency. It works by delivering a precise amount of medical adhesive to the diseased vein, sealing it off and rerouting the blood to other healthy nearby veins.
Sclerotherapy
Sclerotherapy is a minimally-invasive procedure for treating small varicose veins and spider veins. It focuses on closing damaged veins by injecting them with a sclerosing agent, while guided in place using ultrasound imagery. Sclerotherapy is a very common and simple treatment option for varicose veins and spider veins
Surgery
Stripping, for a long time, was considered the most effective way to remove varicose veins, despite the recovery time required. The procedure has been performed for over a century, but has continuously developed with the advancements in medicine and technology.
Treatment Process
Step 01
Initial Consultation
One of our doctors will take a medical history and listen to your concerns. After this, a short scan will be performed letting you know whether you have varicose vein disease.
Your doctor will then discuss your treatment options and plan if necessary.
Step 02
Treatment
Treatments take approximately 45 minutes, are virtually pain free and performed under local anaesthetic. While being treated, you can read, use your phone or request your favourite music to be played. Depending on your case, you may need more than one treatment.
Step 03
Aftercare
After your treatment, you will be required to wear compression stockings, included in your treatment plan, and walk daily.
Most patients find relief of leg aches after treatment. Discover our patients outcomes here.
Before & After
Swipe to see some of the amazing results our patients have had. See more patient outcomes here.



Risks of untreated varicose veins
Venous Eczema
If varicose veins develop, there is a chance that red blood cells which have leaked from the swollen veins will disintegrate. Depositing haemoglobin and other substances into muscle tissue and skin. The result is the skin covering the swollen veins can become irritated and inflamed. This leads to symptoms that start with itching but can quickly progress to tenderness or pain. If untreated, varicose veins can lead to restless leg syndrome or cramping, the development of skin ulcers or thrombosis (blood clots) as well as darkening of the skin around the veins which is known as Varicose Eczema or Stasis Dermatitis.
DVT
Deep vein thrombosis (DVT) is a blood clot that forms deep in the veins, most commonly in the legs. DVT can be dangerous since the blood clots can break away, travel through the circulatory system and become lodged in the lungs – known as a pulmonary embolism.
Phlebitis
Phlebitis is the inflammation of a vein, occurring superficially or deep inside the vein. This condition can result from injury or irritation to the lining of a blood vessel. Superficial phlebitis affects blood vessels closer to the skin, whereas deep phlebitis is found in larger veins, such as those in your legs.
Venous Ulceration
Venous ulcers are large wounds that occur on the skin when faulty valves increase pressure inside the vein. This causes blood proteins and blood cells to leach into the surrounding tissue. If left untreated, this tissue can start to break down due to loss of nutrients and being deprived of oxygen.
FAQ – Everything about varicose veins
What treatments are there for varicose veins?
Are the treatments safe?
Does treatment hurt?
Will I need to take time off work?
What is the recovery plan?
- Minimal to no downtime or time away from work.
- You can drive after the procedure, if you haven’t taken any medications to reduce anxiety.
- No long-distance travel greater than 5 hours is recommended.
- We recommend that all patients wear compression stockings or bandages for a minimum of five days after treatment to assist the healing process.
If there is any discomfort following the treatment the doctor may recommend pain reliever medications.
More questions? Check out our FAQ
























