The biggest aesthetic issue people associate with varicose veins is their twisted, bulging, blue-green appearance. And with summer fast approaching, it’s no surprise that that’s a major concern for some patients. But you might not know that this condition can also negatively affect the skin’s appearance. So, to learn more about how varicose veins affect the skin, keep reading.
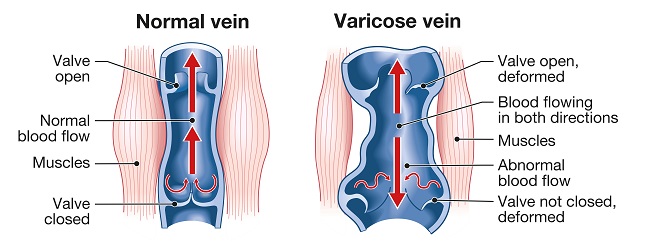
Illustration showing varicose veins and normal veins
Varicose veins are caused by chronic venous insufficiency (CVI). This condition involves the little valves in your veins (responsible for stopping the backward flow of blood) malfunctioning, causing blood to reflux or pool in the vein instead of getting to the heart.
With blood pooling and vein walls expanding, several symptoms start.
- Circulation slows, and capillaries overflow.
- Fluid leaks into surrounding tissue, causing swelling.
- The expanding vein walls agitate surrounding tissue, including the skin.
- And the skin, because of the impacted blood flow, doesn’t get the vital nutrients and oxygen it needs.
How do varicose veins affect the skin?
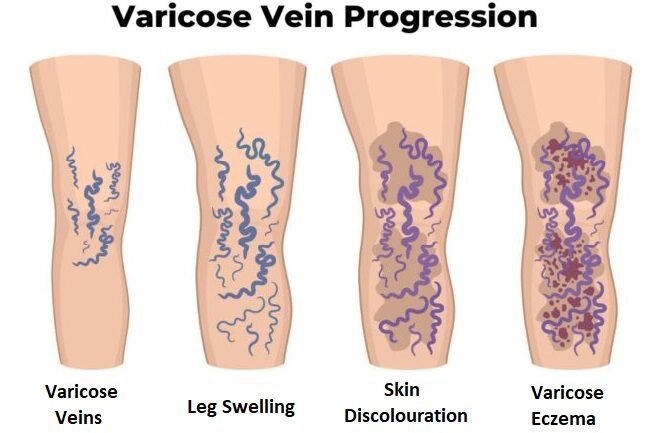
Illustration of the progression of varicose veins on a leg, starting with varicose veins and progressing into swelling, skin discolouration, and varicose eczema
Because of the agitation and nutrient deprivation, your skin can start going through a number of unpleasant changes. These include:
- Inflammation. The skin around the affected area becomes swollen and reddened.
- A shiny appearance
- Discolouration (hyperpigmentation). You may start noticing reddish or brownish patches of skin around the affected area. In the case of varicose veins, hyperpigmentation is not the result of melanin overproduction. Instead, it develops because red blood cells leak out of the vein and into surrounding skin tissue, then break down and ‘stain’ it.
- Stasis dermatitis. Also known as venous or varicose eczema, this stage of skin damage involves the skin drying, thickening, and becoming crusty or scaly. Also occurring due to fluid buildup, this condition is a more advanced and dangerous stage of vein disease. Your skin will become extremely prone to breakage and slow to heal. Hence, it will be prone to infections and may even lead to a venous ulcer, an open skin sore that’s extremely difficult to treat and has a high recurrence rate.
Learn more: How Serious are Varicose Veins
What can I do to reverse these changes?
We know that sounded scary. So, we are sorry to say that hyperpigmentation and stasis dermatitis may become permanent. But. The good news is that proper treatment can improve the appearance of hyperpigmented areas and make eczema-affected skin softer and less prone to damage.
The first step is treating the underlying cause: the varicose veins. Fortunately, several minimally invasive treatment options are available, including RFA, EVLA, Sclerotherapy, ClariVein, and Medical Superglue. So you won’t need surgery.
The next step is seeking out a dermatologist. They’ll provide further advice and treatments, and prescribe medications and topical ointments.
What can I do to prevent them?

Dr Zil Yassine examining a patient’s veins and skin in the treatment room
Another piece of good news is that such skin damage is preventable, provided you take action. If you suspect you have CVI or varicose veins, go to a vein specialist for a proper diagnosis. Even if you don’t think you have either, you should still book a consultation if you’re over 40, have a family history of varicose veins or other venous disorders, went through pregnancy, or smoke.
Additionally, you could make some lifestyle changes to minimise your chances of getting varicose veins or slow their progression into skin damage. These include:
- Eating a vein-friendly diet. Basically, make sure to eat plenty of fruits, veggies, whole grains, nuts, eggs, and fish (if your dietary requirements allow). These foods contain all the vitamins, flavonoids, and omega-3 fatty acids your veins need to stay strong and healthy.
- Be kind to your skin. Wear sunscreen, eat plenty of the foods listed above (because the skin requires many of the same nutrients your veins do), and don’t shy away from moisturisers. Also, see your doctor if you notice any odd changes in skin texture or appearance.
- Get plenty of exercise. Walking, yoga, and swimming are the best workouts for your veins, as they’re enough to get your blood pumping without putting too much stress on the veins.
- Don’t sit or stand for long stretches. When you’re static, your blood flow slows, increasing the chances of reflux. And especially when you’re standing for hours at a time, your leg veins have to fight very hard to get your blood from your ankles to your heart.
- Get compression garments. Medical-grade compression socks are a fantastic investment for your vein health. Especially good for long-haul flights, standing jobs, and strenuous exercise like weightlifting, they’ll gently squeeze your muscles and help tired veins circulate blood out of your extremities.
Seek expert advice
As we mentioned, if you have varicose veins, start experiencing their symptoms, or notice the skin changes associated with them, go to a vein specialist as soon as possible. The earlier we intervene, the better our chances of helping you avoid stasis dermatitis and other unpleasant symptoms and conditions.
So if you’re ready to take action, call us on 0420 102 637 or fill out this form to book your appointment.

