Varicose veins aren’t simply an aesthetic issue. They can be uncomfortable and painful and may lead to more dangerous conditions down the line. The symptoms are often described as an itchy, heavy sensation, sometimes causing a hot or burning feeling. While ultimately the best way to relieve symptoms is to receive treatment, we’ve put together 6 (six) simple ways to relieve vein pain that is bothering you right now.
Why do Varicose Veins Become Painful?
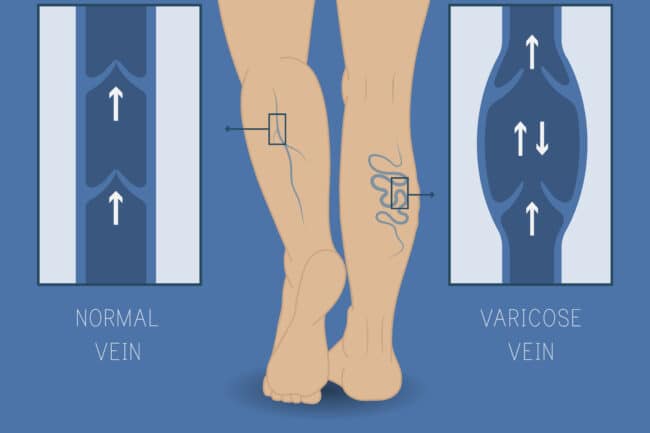
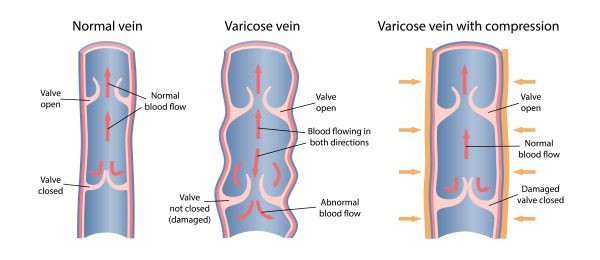
Varicose veins are caused by a condition called chronic venous insufficiency (CVI), which causes the tiny, one-way valves inside the veins to malfunction. These valves stop closing properly, which allows blood to flow back into the veins, and stagnate there. This causes the affected veins to swell, impairs blood flow, and deprives the veins and surrounding tissues of the oxygen and the nutrients they need to stay healthy. Impaired circulation can cause leg tissue to become inflamed, which activates the pain receptors and causes pain.
The types of pain commonly caused by untreated varicose veins include:
- Aching, throbbing discomfort or burning sensations in one of both legs.
- Pain in the legs that becomes worse after standing or sitting tool long.
- Pain when walking of exercising, sometimes resulting in muscle cramps.
- Feelings of heaviness or weakness in the legs, even after rest.
- Itching along the surface of the veins that is so strong that it becomes painful.
- Restless Leg Syndrome, constantly feeling that you have to move your legs to find relief.
Six ways to relieve vein pain:
1. Exercise and stretches
Many of the muscles in your legs act as pumps to help the blood flow back up through your body and up to your heart. The active use of these muscles helps to prevent varicose veins from forming and promotes healthy circulation.
Exercises and stretches that target the calves and ankles in particular help. If you’re sitting or standing for extended periods as part of your work, change position or walk a few steps every 30 minutes. Keeping hydrated assists this process, so make sure you’re drinking plenty of water and minimising diuretics that dehydrate you, like alcohol and caffeine.
2. Clothing and daily wear
The clothes you wear on a daily basis can have a distinct effect on your veins and could be one of the primary causes of vein pain. Tight clothing, especially around your waistline and thighs, can restrict blood flow and cause issues over time. It’s best to wear loose-fitting clothing that’s not constrictive.
Footwear is also important. Whilst high heels might look good, they stop the calf muscles from moving freely and inhibit the pump action that gets the blood moving. Wearing lower-heeled shoes is best.
These actions won’t immediately relieve any current pain but rather work to prevent it from occurring long-term.
3. Diet
Diet again is something that is more about preventing the pain from occurring rather than instant pain relief. This works in two main ways. The first is general weight management. As excess weight puts a strain on the veins in your legs, and in cases of obesity greatly increases the risk of complications.
The other primary way diet can help is by improving the blood circulation itself. This can be done by including flavonoids in your diet. These are nutrient compounds that boost circulation, reduce blood pressure and help relax tensed veins. Foods rich in flavonoids include vegetables like onions, capsicum, spinach and broccoli, as well as citrus fruits, berries, garlic and cocoa.
In both of these, it’s also good to reduce saturated fats and sugars, as these can build up blockages in your veins, causing pain and potentially serious health issues.
4. Compression
Compression stockings are one of the most effective and reliable ways to take care of your veins. They work to effectively reduce and manage vein pain as it occurs, as well as prevent it from happening long-term.
Wearing medical-grade compression stockings, especially during extended periods of sitting or standing like travel, desk work, hospitality and more will greatly help to manage swelling and painful varicose veins.
5. Cold water
The burning and itching pain felt in veins is most commonly caused by blood pooling in the veins, causing pressure on the blood vessels and bleeding that aggravates the surrounding tissue. The best way to alleviate this pain immediately is to cool down the veins and tissue, causing the vessels to stop swelling, reduce inflammation and stop the blood pooling temporarily.
This is best done with a cold shower or a cold bath and should provide immediate relief from the pain and discomfort in your veins.
Learn more: Why do my veins burn?
6. Elevation
This is the easiest way to relieve vein pain as soon as it occurs and can be done virtually anywhere. When you have pain in the blood vessels in your legs, elevating your legs, usually by lying down and raising your legs up on some pillows or a higher piece of furniture, you use gravity to get the blood flowing out of the unhealthy veins and back to your heart. This will help to relieve any immediate symptoms.
While all these methods help to relieve vein pain and reduce the risk of vein problems arising, it’s important to speak to your GP or a vein specialist to look at the best treatment for your veins long-term.
Is it dangerous to leave varicose veins untreated?
Apart from the physical symptoms, which can impede daily life, some varicose veins could lead to other health issues. These include:
- Deep Vein Thrombosis
- Varicose Eczema
- Venous ulcers
- Oedema
Seek expert advice
The doctors at The Vein Institute specialise in varicose vein treatment. We offer patients a comprehensive program using non-surgical laser treatment techniques. To book a consultation and discuss our treatment program, call 13 VEINS (that’s 13 83467) or make an enquiry via the Contact Us page.

